EXTERNAL TRANSPORTATION/PERFORATION AND ITS MANAGEMENT IN A PATIENT WITH COMPLEX MEDICAL HISTORY.
Over the years working as an Endodontist, I was lucky to work in the public dental system for as few years with immense exposure to patients with complex medical histories.
I was intrigued by the nature of complex medical diseases and how I could provided the best endodontic service to my patients as many of them couldn’t afford high end cost of complex endodontic and restorative treatments. Also, some of my patients couldn’t afford to get their tooth extracted due to systemic diseases and risks and medications they were on. This put them is a hight risk category.
I have carried forward my special interest treating patients with complex systemic diseases/medically compromised and hope to put together a few cases that I can share with my colleagues. It is a given that all my patients have provided consent to share there de-identified radiographs for the purpose of dental education. I am still not sure if I am ready to share clinical photographs on social media but I will make a start here.
Not all endodontic treatment is about white lines running and there is more to a tooth as it is a part of the periodontium that is further a part of the jaw/head and neck and our body. I like to look at my work more holistically and what I can provide for my patients by trying to retain a tooth and in the process help heal the apical disease or pain associated.
A lovely courageous lady, mother of few young children with complex medical issues including moderately controlled diabetes, dental phobia, previous heart conditions and taking I/v bisphosphonates since the past 5 to 6 years for previous cancer and ongoing osteoporosis etc. Now you may think what is all this to do with Endodontics? The answer is I am not sure as the research has not caught up with complex clinical work but what ever literature and regulations/position papers are available, I know that I have no choice but to retain her teeth due to a high risk of MRONJ (medication related osteonecrosis of the jaw). I will discuss the relationship of Endodontics with CVD and diabetes is another post or atleast what I make of it.
Teeth 36 and 37 diagnosed with irreversible pulpits due to possible cuspal cracks. Pulp extripated by her dentist and referred to me for continuation due to complex root canal morphology.
I decided to treat both the teeth together to save time as my patient has far bigger issues and worries to deal with in her life than just a getting her teeth fixed. Nevertheless, this was important as there was no alternatives and extraction was out of question. I managed to locate all canals but something didn’t feel right while negotiating the distal canal #37. I wasn’t getting the right tactile feel as I should. I took a radiograph as there it was, a Perforation, mid to apical root on a moderately curved canal that was extremely thin as well.
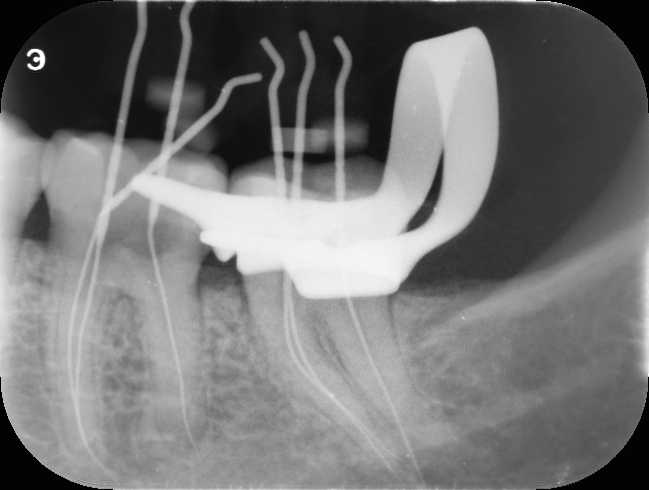
I had no other choice but to keep trying, I was aware that she is taking bisphosphonates, she is also a diabetic with previous history of CVD. I had to be gently not to lacerate/injure the periodontium and also get back into the canal. An external transportation close to the apical 3rd is very difficult to manage even with the microscope and the best illumination as you cannot see past the curvature.
It took me 2 separate appointments, with multiple attempts and pre curving my S S K file/pilot files right from no 6 to 10 but I eventually got back into the canal.
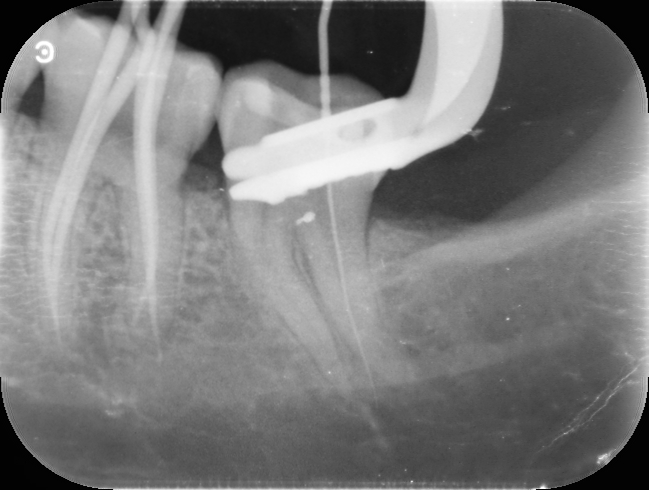
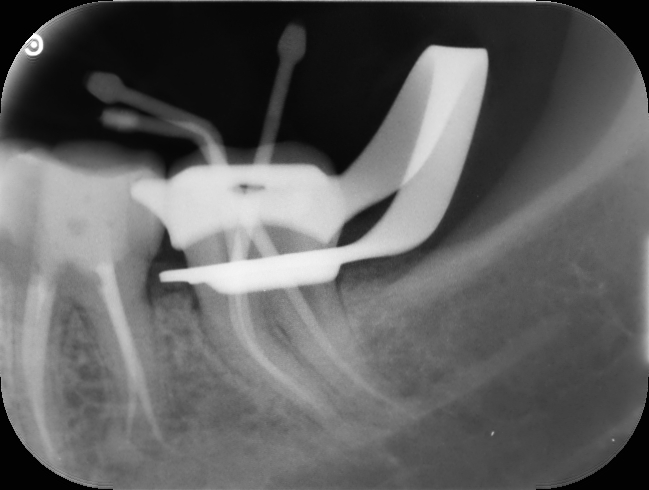
Now sealing a perforation that apical is again very difficult. The best material for this is a bio ceramic Root repair material. A flowable injection technique with a thin long tip. There was no way to get MTA in there. I anyway have been slowly moving towards using bioceramic materials rather than using MTA for everything. MTA does have its place but now we have alternatives that can be handled and managed better.
Thin white line mesial to the distal canal from the middle 3rd shows the sealing of the perforation #37

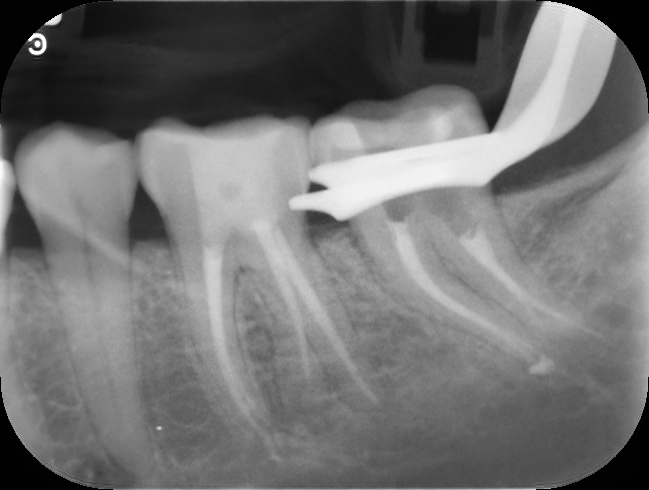
3 month followup with no signs or symptoms. Referred back for onlay/crown
I was lucky to be able to fix this successfully but there is nothing like prevention. What steps should we take to prevent something like this?
- Study the root canal morphology by taking a couple of PA radiographs during the consult appointment.
- If you cant find the orifices, you possibly need to refine your access preparation. I don’t mean that you keep enlarging it but only refine it so your access isn’t compromised. You don’t need to follow the ninja and ultra conservative access preparations if you are not be able to access the canals and debride/clean them appropriately.
- Always negotiate canals with K files either 8 or 10. No 6 is a difficult file to manage as you may break it easily, so be cautious.
- Only when you have accessed the canal to length with no. 10 file should you consider moving to rotary.
- Don’t apply any pressure or force. It is all about gentle negotiation and not rushing.
- Focus, remain steady and breathe
More coming soon. Please feel free to leave your comments and queries. I would love to hear from you.
3 Comments
Leave a Comment
You must be logged in to post a comment.
Thank you for presenting such a complicated case and your honesty in dealing with the perforation
Just a question if CBCT would have helped in locating the perforation quicker?
I have come across dentist from the US that routinely take CBCT if they are treating molar teeth
Would this make a difference?
thanks
Hello Chandy,
Thank you for your interest in this case.
It was indeed an interesting one.
CBCT is fast becoming a standard of care in endodontics especially complex cases. This cases would have benefited a bit from CBCT but luckily I could visualize the perforation through my scope and could locate the real canal path. Not always possible.
This patient was pregnant at the time so I couldn’t take the CBCT or I would have.
In general, about 60-70% endo cases I see undergo CBCT during assessment in my practice and I find this number increasing constantly.
Thank you for posting such a wonderful article. It helped me a lot and I adore the topic.